- Building a Sustainable QI Network at BC Children’s Hospital
-
Three pediatric physicians at the BC Children’s Hospital have a long-term vision to create a BC Pediatric Quality Improvement Practitioners (BCPQIP) Network. It brings physicians who have an interest in QI together on a regular basis to network with QI colleagues, share knowledge, receive guidance/advise and help further spread QI work.
Drs Tiffany Wong, Mia Remington and Sandesh Shivananda have all participated in QI in various ways, including through SSC’s Physician Quality Improvement (PQI) program.
Although there was a lot of QI work being done in the hospital – much of it was siloed. “We came together in a very organic way,” Dr Wong says. “Mia and I met through PQI and we met Sandesh through his work with the Hudson scholarship program, which is a program that allows junior physician scholars to focus on quality improvement one day a week over a two-year period.”
. .

Left to right: Drs Tiffany Wong, Mia Remington and Sandesh Shivananda
Moving from silos to collaboration
Drs Wong, Remington and Shivananda acting as co-chairs began to build the network with funding from SSC’s Facility Engagement Initiative and Health System Redesign. They reached out to Quality Leads within each hospital division, physicians who have participated in PQI, Hudson scholars and others who expressed an interest in QI. Dr Remington notes, “We conducted a needs assessment survey before our first meeting because we didn’t believe the three of us should be setting the direction – it’s a shared experience.”
The survey responses helped to guide their first meeting in October 2020. There were about 27 physicians who all weighed ideas, expressed opinions and helped set priorities. Of course, all of this work was happening at the height of the pandemic, so Zoom meetings were core to furthering the development of the network.
Learnings from the survey and first meeting found that physicians wanted regular quarterly 90-minute meetings to share and receive feedback from QI colleagues on their projects, hear from QI experts and create partnerships for the spread of QI work across hospital programs. Physicians also wanted to foster engagement with the Health Authority (HA) Leaders and create a QI centre of excellence with ongoing operational funding. The co-chairs then prioritized their next steps.
The initial intention was to have the FE funding pay for speakers and some meetings held in a semi-formal atmosphere for face-to-face and network opportunities – but pandemic restrictions eliminated this approach. Two of the co-chairs went to the Institute for Healthcare Improvement (IHI) Annual conference in 2020 and identified some outside speakers, who they invited to present to the BCPQIP network. There have now been regular quarterly meetings held all through 2021 on Zoom with full attendance.
Dr Claire Seaton joined the network and says, “working in QI lends itself to collaboration, learning from others’ successes and failures, and getting feedback. The network gives us a space to do this, and has supported our efforts to be recognized for our work. I’m grateful to be a part of it.”
“We had a couple of HA Leaders invited to our meetings including Dr Felicia Lang, who is a Quality Lead within the health authority," Dr Remington notes. "She spoke to our group around quality structures – so it was a good opportunity to get to know each other.”
The next meeting is in April and for the first time it is planned to be a face-to-face dinner meeting with the goal of setting their direction for the coming year. Health Authority Lead Dr Derek Human is scheduled to share his experiences in QI, and also help members identify HA quality improvement initiatives that could be of interest to them.
“We don’t pay anyone to come to our events and they still come. I think they see value in being connected with like-minded colleagues,” he observes. “I think that is really powerful and valuable in itself.”
Success factors: connections, relationships
The co-chairs agree that to be successful you need to really use your network, identify champions, and make meetings valuable so people want to attend.
Dr Shivananda notes, “We started this journey by nurturing connections and relationships between members. One of the challenges faced by our physician leaders is maintaining enthusiasm in driving change. Validation and appreciation of their efforts by peers helps everyone be resilient and remain engaged.”
Since the network has been established there have been a number of diverse QI projects presented and discussed, including a multi-disciplinary approach to asthma education, prescription medication equity and a parenteral nutrition program.
In addition, Dr Wong worked with the Faculty of Medicine DARPT committee to develop a promotions package where a doctor could be promoted based on QI work from Clinical Instructor right up to Full Professor.
“We developed a package with the DARPT committee and presented it to the pediatrics department,” she said. “They liked it so much they brought it to the Faculty of Medicine. After some revisions, it has been formally accepted. I’m very proud that health quality improvement, systems innovation and patient safety work is now formally recognized as important academic work.”
QI work will continue to be integral to delivering quality patient care and the BCPQIP Network is laying the groundwork for sustainable QI improvements in BC. Dr Shivananda is optimistic about the future. “We hope to strengthen the infrastructure for spread and scalability of innovative practices across the campus and beyond."
This work has been supported with funding from the Specialist Services Committee Facility Engagement Initiative and Health System Redesign. Both are joint initiatives of Doctors of BC and the Government of BC.
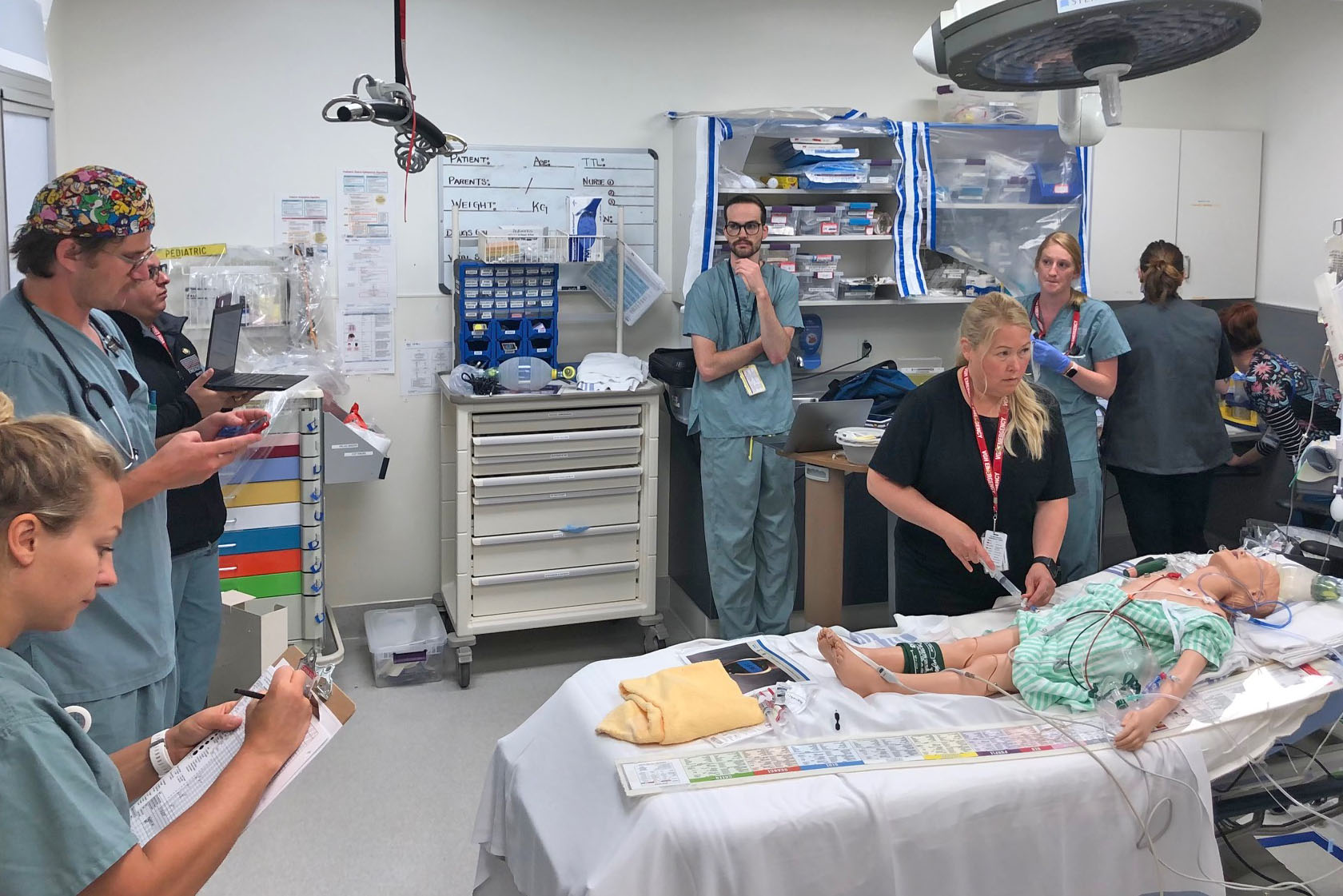
When the ‘heat dome’ descended recently onto British Columbia, many emergency departments were flooded with patients suffering from a dangerous condition known as hyperthermia.
Fortunately, Victoria-based Emergency Department (ED) physicians had run a hyperthermia scenario a year prior through its ED Simulation initiative, and identified important gaps in care that could be remediated. These included having ready access to cooled-IV fluids, body bags that could be filled with ice and water to further cool patients, and fans for misting.


 These are challenging times in BC, and staying positive is more important than ever.
These are challenging times in BC, and staying positive is more important than ever.
 Martin explains that traditional cleansing ceremonies have been used by her ancestors for generations and continue today. “
Martin explains that traditional cleansing ceremonies have been used by her ancestors for generations and continue today. “ “A First Nations Cultural Worker came to the hospital to do a cleansing ceremony for some patients,” he says. “We didn’t see any of those patients for more than a year after. When I would see them in the community, I could see they were doing better. That is hard to ignore."
“A First Nations Cultural Worker came to the hospital to do a cleansing ceremony for some patients,” he says. “We didn’t see any of those patients for more than a year after. When I would see them in the community, I could see they were doing better. That is hard to ignore." Chris Seitcher has worked in the helping field for many years, including as a care aid with Island Health, and for elders in the Tla-o-qui-aht
Chris Seitcher has worked in the helping field for many years, including as a care aid with Island Health, and for elders in the Tla-o-qui-aht
 Over time, the aim of those involved is to introduce traditional healing practices more widely with health care professionals, ambulance crews, firefighters, the coast guard, and police officers—all of whom are exposed to emotional and physical trauma—and to create stronger cultural connections among patients, health care, and emergency professionals.
Over time, the aim of those involved is to introduce traditional healing practices more widely with health care professionals, ambulance crews, firefighters, the coast guard, and police officers—all of whom are exposed to emotional and physical trauma—and to create stronger cultural connections among patients, health care, and emergency professionals.



