- 2020 Facility Engagement (FE) Evaluation Survey
-
- Coronavirus (COVID-19)
-
During the COVID-19 situation, Facility Engagement MSA project teams are encouraged to stay in touch with your Facility Engagement Liaison (FEL) about short-term and ongoing work and supports related to FE. Please see MSA activities related to COVID-19, COVID FE Funding Best Practices and Doctors of BC COVID-19 resource page.
- What is changing?
-
A lot has changed in the four years since the Specialist Services Committee launched Facility Engagement across BC to strengthen meaningful physician involvement in health authority decision-making.
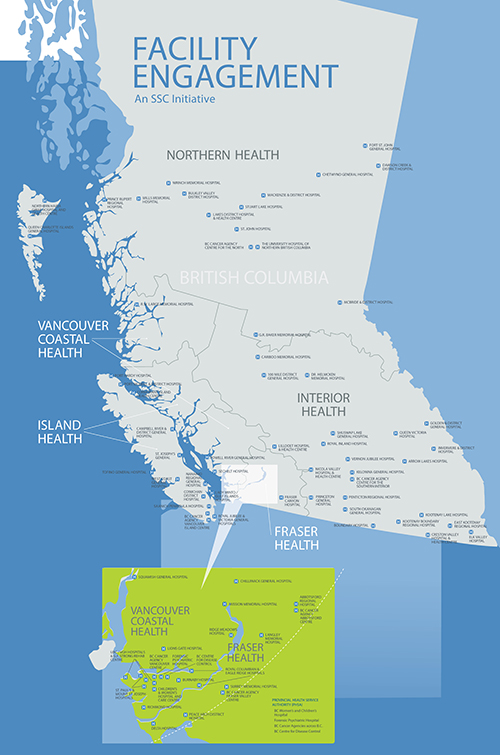
- Across BC’s acute care facilities and programs, 72 Medical Staff Associations (MSAs) in 6 health authorities have galvanized more than 4,300 physicians to participate in 2600+ Facility Engagement activities. (Updated to February 2020).
- A combination of new structures, funding, physician leadership, and administrative supports are enabling MSAs and their physician members to improve engagement and teamwork among colleagues and with health authorities, in ways that were not possible in the past.
- The UBC evaluation of Facility Engagement to March 2019 found that medical staff and health authority leaders think that participation in the initiative is worthwhile.
With all of this activity – and a lot of hard work – a sense of optimism is fueling a growing culture of engagement across BC, with renewed teamwork and positive experiences reported by many of those involved.
Big themes: Foundation for change
“This is an exercise in relationships – setting a foundation that allows us to grow as an organization, as people, as a team, as partners in care.” – Dr. Harsh Hundal, Executive Medical Director Physician Engagement & Resource Planning, Interior Health
-
Physician-to-physician communication and relationships are improving as a key step for MSAs to build a strong foundation for engagement and a medical staff voice. Physicians are connecting and meeting across sites and regions – for the first time ever in some cases – to get to know and support each other, discuss priorities and work on projects that strengthen their hospital, patient care, and personal well-being.
-
Communication with health authorities is improving. At many sites, MSA working groups and physician members are regularly meeting and establishing collaborative processes with health authority administrators and leaders to discuss respective priorities, and to work on projects together.
-
Physician wellness has also surfaced as a priority, with MSAs across BC initiating activities that aim to reduce the risk of burnout and support physicians to provide patient care in a healthier way. Some MSAs are now starting to elevate these efforts to an organizational, regional and system level to look at potential improvements that can reduce the risk of burnout. (Doctors of BC is further working on this priority through the Physician Burdens engagement and policy development process.)
-
With the new 2019 Physician Master Agreement, Facility Engagement is also officially supporting medical staff engagement in the implementation of electronic health records, starting with Lower Mainland hospitals that are adopting the Cerner syste
Moving Forward
There is more work to be done to achieve sustained change, and further evaluation of the Facility Engagement Initiative will to measure its ongoing impact. Meanwhile, both physicians and health authority partners from many parts of the province report they are making headway to build trust and to make decisions together that impact their hospitals, programs, work culture and patient services. Stay tuned as this great work continues to unfold!
Read examples and successes > www.facilityengagement.ca/stories
- Across BC’s acute care facilities and programs, 72 Medical Staff Associations (MSAs) in 6 health authorities have galvanized more than 4,300 physicians to participate in 2600+ Facility Engagement activities. (Updated to February 2020).
- Courage and community come together to improve surgical quality and safety
-
Dr Michel Hjelkrem, an orthopedic surgeon at Kootenay Boundary Regional Hospital took what some might consider drastic steps to reduce surgical site infections – he stopped doing joint replacements. Then his four partners joined him. For the next two and half months, they embarked on a mission to collaborate with their health authority to improve surgical standards. And while it wasn’t always an easy road, it turned out to be one of the best decisions they made to lower infection rates well below the national average.
- Physicians Advocating for Wellness
-

Physician health is a common theme for MSAs, with 100+ wellness-related activities underway across BC. They range from group fitness to social opportunities, to relationship-building across medical disciplines, to tackling workplace and system frustrations. The engagement of physicians in a health care organization is, in itself, a key factor to reducing burnout.
The FE provincial team is looking at how to coordinate MSA physician wellness activities with other regional / provincial efforts including those of Doctors of BC. As a start, new FE funding guidelines for physician wellness have been introduced to elevate physician health activities to a strategic level moving forward. Find them here under 'funding.'>
Meanwhile, last November, Fraser Health’s regional Medical Staff Wellness Committee welcomed 45 physician health champions from its 12 hospitals and 10 divisions, as well as health authority leadership, to brainstorm how Fraser Health could support and promote physician health. As their ideas unfolded, the Committee realized that they were sowing the seeds for a regional Physician Health Program. Read about it here >
- Physicians: How are you interacting with your hospital and health authority?
-

Doctors of BC's annual Physician Health Authority Engagement survey is here! BC physicians and specialists are invited to answer a 3-minute survey to provide important insights about how MSAs can advocate for physicians within our facilities and the community and to create and focus programs and policies to better support physician work with health authorities.
Anonymous. Confidential. Deadline: April 30, 2019.
- To complete the survey, look for the invitation sent to your e-mail from Health Standards Organizationon April 1 with reminders thereafter. (Screenshot of invitation is below).
- Can't find the e-mail invitation? Ask for one at surveys@doctorsofbc.ca.
- Reconnect with meaning and purpose
-
Trusted expert and internationally recognized caregiver advocate for reducing clinician fatigue and improving employee engagement, Dr. Stephen Swensen, Professor Emeritus, Mayo Clinic, met with members of the Vancouver Physician Staff Association this January. He shared lessons learned over his three-decade-long career with the Mayo Clinic.
“Many physicians are working in a state of professional distress,” stated Dr. Swensen. “This goes beyond burnout and includes PTSD, emotional exhaustion, clinical depression, moral injury, compassion fatigue, and suicidal thoughts. When you’re in this state, you’re more likely to make a medical error. You have relationship problems, addiction problems; your productivity goes down as does your level of quality of care. One of the biggest opportunities we have to improve patient care is by caring for each other.”
An ideal workplace has three elements that Dr. Swensen calls agency, coherence and camaraderie. The happiest teams at the Mayo Clinic, he said, have the agency to make decisions, feel connected to their group, and celebrate each other’s milestones.
Leadership behaviours
Dr. Swensen identifies five behaviours (Leader Index Behaviours) that make for better leaders:
- They are inclusive.
- They communicate transparently.
- They value your ideas.
- They are interested in your career.
- They appreciate your work.
Mayo Clinic staff are surveyed annually on how their leaders rate in these areas. Those with low scores are coached to improve these or are moved out of leadership roles because leaders who don’t exhibit these five behaviours are causing harm to patients.
Medicine is a calling
Some people go to work every day for the paycheque; others see their career as a means to accomplish goals and receive acknowledgement of their contributions. It is common for those who choose a career in health care to also see their work as a calling, as a means of helping patients, their families and the greater community. When that sense of purpose is lost, said Dr. Swensen, physicians can develop professional distress.
“Engagement is the antipode to burnout; it connects us to meaning and purpose,” he said. “The number one driver of happiness is meaningful work so you would think health care should have the lowest rate of burnout. But sometimes we lose sight and have to be reconnected to our purpose. Coherence can do that. Coherence exists when all parts of the system fit together to form a united whole.”
To create coherence, leaders need to ask, listen and empower.
“It’s that annoying pebble in your shoe that holds you back rather than the mountain you need to climb. The research is clear that when departments work together to identify the ‘pebble’ they reduce burnout. You can apply this to Cerner. Superusers could monitor who’s using the system on weeknights and weekends and then ask them if they need assistance. A superuser can save a physician three to five hours a day by teaching them shortcuts.”
Architects rather than carpenters
The pronouns we use when we talk about our organization are a clue to how well that organization is thriving. When we think in terms of ‘us’ and ‘them’ rather than ‘we’ and ‘our,’ the institution flounders.
“If physicians are treated as partners, they behave that way,” said Dr. Swensen, who recalled how the Mayo’s chair of haematology addressed her team’s high burnout rate.
“She decided to be a leader, a champion—rather than a middle manager. Instead of saying this is what they’re telling us to do, let’s all just be carpenters, she empowered her physicians to be architects. They weren’t going to be told how to do something by people who don’t understand what they do. The team created the solutions.”
When we do our work, improve our work, and care for each other, our patients have the best doctors imaginable. Lean into tomorrow, Dr. Swensen encouraged, to see what difference you can make.
Further reading: Finding and Creating Joy in Work white paper (IHI white paper, co-authored by Dr. Swensen)
Thank you to the Vancouver Physician Staff Association (VPSA) for sharing this article and photos. >
- Saving the Elk Valley Hospital Operating Room
-
Little did they know that the retirement of their only general surgeon at Elk Valley Hospital (EVH) in Fernie would bring about a significant opportunity for collaboration with both the physicians in the neighboring community and their Interior Health partner.

Having no luck with recruiting a new specialist surgeon for the hospital, despite a strong partnership with local governments to assist the recruitment efforts, physicians and staff started thinking about what could be done to save the OR. After all, this retirement could mean that surgical services in Elk Valley Hospital would have to close down and over 15,000 residents in Fernie, Elkford, Sparwood, Elko, and Jaffray would have to travel as much as 170 km to the nearest hospital in Cranbrook both for consultations and surgeries. Road conditions during the winter could make it even more challenging for patients to receive surgical care, especially for pregnant mothers requiring a C-section. Increased pressure on hospital staff and resources in Cranbrook from the additional elective day surgeries could also lead to longer wait times in that community.
In order to identify a solution that would save and sustain the OR in Fernie and not destabilize OR services in Cranbrook, physicians came together through funding from Facility Engagement to create a Surgical Sustainability Committee. The committee included representation from the physicians and Interior Health Authority (IHA) including the Chief of Staff, Health Services Administrator, Health Services Director, Site Manager, Medical Administrative Assistant, and Patient Care Coordinator (head nurse).
The solution conceived was both creative and sustainable, and involved the engagement of all parties. First, a Family Practitioner with Enhanced Surgical Skills (FPESS) was recruited to regain a slate of elective day surgeries in Fernie. However, as the FPESS was not starting for 12 months, the committee reached out to the Surgical Unit at East Kootenay Regional Hospital in Cranbrook, the neighboring city, to discuss an opportunity for them to perform surgeries at Elk Valley Hospital - with a goal of meeting patient needs closer to home while creating an opportunity to add sustainability to both surgical programs.
Through one-on-one personal phone calls made by committee members, specialist physicians in Cranbrook were able to discuss the opportunity and express their interest formally. EVH Physicians attended a Surgical Leadership meeting in Cranbrook to present the opportunity at their rural facility, and build their relationship with the Surgical Specialists.
Cranbrook surgeons were provided with all relevant information for working at Elk Valley Hospital, including the OR schedule of open days, an offer to have Fernie nurses travel to Cranbrook for a day to observe the surgeons’ working styles to build mutual comfort levels, and coverage of travel costs for surgeons through Northern and Isolation Assistance Outreach Program (NITAOP).In addition, an examination room was secured at Elk Valley Hospital for patient consults and equipped with furniture, donated local artwork, a fridge, and a nespresso machine to serve as a comfortable ‘home away from home’ for visiting surgeons as a model consultation space and a comfortable private space to take breaks between surgeries.
On the first day of work, Elk Valley Hospital staff and physicians came together for lunch sponsored by Facility Engagement to welcome and meet the visiting surgeons. Jacqueline Arling, the Facility Engagement Project Manager for Elk Valley Hospital, believes that the key to this solution was relationship building. “A big factor for the surgical sustainability success is that physicians have built trust and relationship with both the Cranbrook physicians and Interior Health.”
The residents of the Elk Valley now have four visiting general surgeons conducting consults and surgery at the Elk Valley Hospital, in addition to the current GPs and soon-to- start FPESS physician. The surgeons are proud of being able to help a neighboring community in need of specialist care. Taking collaboration to yet another level, these surgeons can also help mentor the local FPESS to expand their capabilities to perform surgeries in Fernie.
Reflecting on the success in Fernie, Karyn Morash, Health Services Director said, “With the advent of Divisions of Family Practice and Facility Engagement the way physicians were coming to the table was changing, it facilitated our ability to work more closely together.” while noting that “to the health authority’s credit, we have worked with determination to honor our part of the commitment to engagement with MSAs.”
Given the historical communication challenges that existed between health authorities and facility-based physicians, Elk Valley Hospital is a perfect case example of solution finding made possible through collaborative efforts leading in turn to improved patient care--the ultimate goal of the physicians, health authority and the Facility Engagement Initiative.
- Facility Engagement Funding Guidelines
-

One theme expressed by MSAs both at the March mid-term site review meeting and through the recent interim UBC evaluation is the need for clarification around the MOU funding criteria. Supplementary funding guidelines were recently approved at the June meeting of the SSC Facility Engagement Working Group (FEWG). Over the next 6 to 12 months, the FE team will monitor feedback from the HAs and MSAs over the use of the guidelines and report back to the SSC FEWG on any substantive input and/or recommended changes. Read the full guidelines here.
- Facility Engagement Provincial Evaluation
-

A team of researchers from UBC has come together to evaluate the Facility Engagement Initiative and the implementation of the Memorandum of Understanding on Regional and Local Engagement (MOU). The provincial evaluation will:
• take place from now to early 2019;
• provide real time feedback about the implementation of the initiative which can be used for immediate improvements;
• gather evidence to understand and measure the success of Facility Engagement activities; and
• provide accountability to all stakeholders.Physician societies and health authorities will receive a package of information shortly outlining when and how to participate in the provincial evaluation. Read more here >
- Alcohol Policy
-

The Ministry of Health has advised that any funding provided via the Physician Master Agreement cannot be used to purchase alcohol. This covers all collaborative funding including SSC Facility Engagement funding for Medical Staff Associations’ (MSAs) operations and activities. Read the full policy here.
- Private Vehicle Mileage Reimbursement Policy
-

Doctors of BC has recently changed its policy regarding the use of private vehicles for work travel, and we would like to communicate this update to all sites. It is recommended that MSAs/physician societies follow these guidelines to provide consistency as they develop their own policies around private vehicle travel reimbursement.
The Doctors of BC reimbursement rate matches the Ministry rate and is pre-set in FEMS (e.g., $0.53/km).
- What is FESC?
-

Facility Engagement Services Company (FESC) is a new legal entity for unincorporated MSAs (smaller sites) to manage funds and contracts, and limit liability risk for MSA executives. FESC will support your MSA with regards to cost-effectiveness, local autonomy, reporting, managing and sessional claims as well as funding and accountability. Your Facility Engagement Liaison (FEL) will discuss this new structure with you.
- New Facility Engagement Sites
-

As the Facility Engagement Initiative is growing, so are the number of sites working with us. Congratulations to the seven sites approved for full FE funding in 2018 so far. The number of fully funded sites has now reached to 59!
- Arrow Lakes Hospital
- Dr. Helmcken Memorial Hospital
- Nicola Valley Hospital and Health Centre
- Prince Rupert Regional Hospital
- R.W. Large Memorial Hospital
- Sechelt Hospital
- St. John Hospital
- Data Driven Improvement Workshop
-

“The Data-Driven Improvements workshops held by the BC Patient and Safety Quality Council provided attendees with practical and applicable strategies to drive healthcare program improvements. Content included effectively identifying indicators, efficient data collection, and practical analysis techniques. This is a great workshop for those seeking to achieve project goals and assess project success.” – Workshop Attendee
Click here for upcoming workshop dates.
- FEMS Quick Tips
-

With Delta Hospital and North Island Hospital Comox Valley now fully operational in FEMS, we’re so pleased to announce that our onboarding of all 27 incorporated physicians societies is complete. With over 2500 members, FEMS has processed over $6M worth of claims for the Facility Engagement Initiative.
Our next step is to bring the MSAs that are not incorporated on board. This will take place in the fall, with regional training sessions and refreshers being offered around the province by Maria Chessari, our new FEMS Project Coordinator. We have taken this opportunity to include a few improvements to this release version:
- Updated column titles and button names
- Grids and filters with improved functionality
- More user friendly reports generator allowing for detailed reporting on multiple levels.
If you have any questions or concerns about the changes, please reach out to our team at FEMS Support by contacting us at femssupport@doctorsofbc.ca, 604-638-4869, or 1-800-665-2262.
- MSAs share experiences and support needs at spring check in
-
On March 6, 2018, physician groups from across BC and the Specialist Services Committee’s Facility Engagement Working Group (SSC FEWG) met to review site activities, a work plan and funding needs for 2018/19. It was a valuable and necessary step to identify local needs and challenges that can be supported and addressed by regional and/or provincial strategies.
The initiative is the first of its kind in Canada with no models to draw on. After hearing about experiences on the ground, the SSC FEWG can make informed decisions with greater clarity for the benefit of local sites.

Some common themes heard on March 6
Funding Guidelines: Some sites feel challenged to allocate funds and would like more direction around funding guidelines. There continue to be grey areas, and activities don’t always appear to be linked to engagement. Some physicians, rural areas in particular, have enough funds but little time to execute projects – so want flexibility to deploy funding more creatively to have more staff to work on projects and reduce the administrative burden. Hearing about these needs and the examples of activities is informing the work of the SSC FEWG to develop funding guidelines in 2018.
Physician Engagement: Overall, sites reported that greater numbers of physicians are joining working groups and getting involved in projects. At many sites, the revitalization of physician lounges has been key starting point to ensure physicians have a quiet, dedicated space where they can meet and interact with colleagues.
While funding is a welcome support, physicians have limited time to participate, or carry out activities. Burnout is a concern. To address this, many sites starting to engage more physicians to be involved in committees and events, and to expand representation from a few select champions.
Health Authority Relationships: MSAs are in various stages of strengthening relationships with their health authorities, and some are reporting great success. Many sites have shared work plans and invited health authority / site representatives to join working groups. In some cases, coordinating data gathering from health authorities to inform the work has been challenging, and sites would appreciate help on that front.
Provincial Supports: Facility Engagement Liaisons (FELs) were seen to be providing excellent support. Support for the Facility Engagement Management System (FEMs) has been useful. However, challenges still exist around getting physicians registered to use FEMS and concerns about the administrative burden of FEMs, especially at smaller sites. The FEMS technology is continually being enhanced to improve the experience.Overall, the great work and plans presented by all sites are exciting, and momentum is building in the right direction. Thank you for your efforts and participation in this process, and continued work to make a difference for your physician colleagues, patients and hospital sites.
- Facility Engagement: Relationships Drive Change - Dr. Sam Bugis
-
My father, who was an obstetrician, worked at the tertiary care teaching hospital in Edmonton. He used to say he would frequently see Dr Snell—the CEO of the hospital at the time—in the hallway. If there was an issue to discuss, the two of them would just talk about it. Today, doctors may never see the CEO or other senior executives. Read more >
- Facility Engagement Liaison (FEL) and Regional Advisor and Advocate (RAA) roles
-
How do the roles of Facility Engagement Liaisons (FELs) differ from Facility Engagement and Regional Advisors and Advocates (RAAs)? Read this description to learn more about how the two roles differ in terms of primary duties, day-to-day examples, oversight, team make-up and out-of-scope duties.
- Physician Burnout Challenge Explored
-
Physician burnout was the topic of a recent Doctors of BC event, hosted by Dr Andrew Clarke, Executive Director of the Physician Health Program (PHP). Attendees included close to 50 physicians representing medical staff associations (MSAs) and divisions of family practice. For Dr Clarke’s brief summary of the background, intention, and goals of the session and the PHP, read “Helping to meet the challenge of physician burnout.”
- New on the Facility Engagement Website
-
New Resources Available: www.facilityengagement.ca/your-facility/need-tools-and-resources
- Doctors of BC Sessional Rates
- Budget Builder Template
- Society Director Compensation
- AGM Documents:
- Maintaining a Society Information page
- AGM Agenda Template
- AGM Minutes Template
- AGM Notice Template
- AGM Planning Tool
- Report to Directors Template
- AGM Presentation Template
- FEMS Quick Tips - May 2018
-
Physician Sessional Rate Increase: April 1, 2018
Effective April 1, 2018, the sessional rates for physicians increased. When submitting claims in FEMS, please make sure that you select the correct date in the ‘Date of Activity’ field. Your sessional rate is dependent upon the date you participated in the activity, not the date you are submitting your claim.- Specialists: As of April 1, 2018 - $157.79 per hour
- GPs: As of April 1, 2018 $133.77 per hour
Financial Interface (for incorporated sites) Reminder:
A reconciliation process should be performed monthly to ensure that FEMS and your accounting software are balanced and up to date. See the guidelines here starting on Page 17, item 5. >FEMS Updates: As part of the commitment to increase user experience and functionality, some changes have been incorporated into FEMS:
- Claim reviewers will be able to adjust the date of activity when reviewing a claim.
- Engagement Activity (EA) Authors will be able to delete Engagement Activities that were set up in Error, and are in Draft status.
- Claims grid will be updated to show the date of activity of the claim, as well as when it was submitted.
VersaPay functionality and security reminder: VersaPay is a third party payment processor that administers electronic fund transfers for claims submitted in FEMS. Canadian-based, it has been vetted by Doctors of BC’s legal counsel and is compliant with the Payment Card Industry requirements for hosting banking information.
The recipient of funds is the only person with access to the banking information provided to VersaPay. A bank account cannot be debited without express consent. During initial validation, Versapay will deposit and withdraw the same small amount to and from the account. This 'micro credit /debit' step is standard industry practice also used by PayPal and other processors.
- Momentum Grows into 2018
-
As of 2018, 69 physician groups from across BC have initiated more than 500 Facility Engagement activities. Thanks to everyone’s contributions – both MSAs and health authorities – physicians are gaining a stronger voice and increased opportunities for meaningful involvement in decision-making.
Activities are renewing relationships among physicians and medical staff. “The MSA has never had an AGM before and there was generally low attendance at meetings. Through the engagement survey process, communicating with physicians about the active role of the MSA/Royal Inland Hospital Physician Association (RIHPA) in supporting physicians, and conducting a CME needs assessment, we were able to re-invigorate the MSA membership. Our AGM was a huge success with 90+ people in attendance. We had Interior Health guests present and there was very positive discussion about the ongoing engagement efforts; including a number of positive comments about RIHPA and the changes seen with regard to engagement of the medical staff over the past year.” (Royal Inland Hospital)
 Collaboration between medical staff, hospital administrators and health authorities is growing. “A 'no secrets-no surprises' philosophy was developed whereby all MSA activities were communicated to the hospital's operational and senior leadership at the project conception stage. An element of trust was created, as we became mutually responsive to priorities of the hospital and of the physicians. The willingness of the hospital executives to collaborate allowed physicians to feel that there is no area of operational management that is off limits to physician engagement… This culture change has led to our physicians having greater confidence in their ability to make change.” (Ridge Meadows Hospital)
Collaboration between medical staff, hospital administrators and health authorities is growing. “A 'no secrets-no surprises' philosophy was developed whereby all MSA activities were communicated to the hospital's operational and senior leadership at the project conception stage. An element of trust was created, as we became mutually responsive to priorities of the hospital and of the physicians. The willingness of the hospital executives to collaborate allowed physicians to feel that there is no area of operational management that is off limits to physician engagement… This culture change has led to our physicians having greater confidence in their ability to make change.” (Ridge Meadows Hospital)
Read more reflections and examples from sites and health authorities at: www.facilityengagement.ca/stories
- MSAs and Health Authorities Share Perspectives
-
A number of ongoing regional workshops and meetings have created opportunities for physicians, health authority leaders and project teams to meet face-to-face to discuss ways to improve trust, collaboration and communication – and to identify common issues, opportunities and next steps. They have been well-received as a great way to share and learn from other's experiences. Perspectives from some of the meetings to date can be found at the links below.
- Island MSA Facility Engagement Event– November 25, 2017: 9 MSA executives, 12 site project and administrators, 3 health authority representatives.
- Fraser Health Workshop – November 29, 2017: 24 physicians and health authority leads from 12 hospitals.
- Interior Health Symposium – December 6, 2017: 53 participants from 17 sites, including a physician representative from each IHA facility, IHA health administrators and executive.
- Physician Wellness Event: April 3
-

SAVE THE DATE: April 3, 2018
As awareness of physician burnout increases, physician health and wellness initiatives are becoming a strategic priority for many medical staff associations. To support physician groups who wish to improve the psychological health and well-being of their members, the Physician Health Program will host a one-day session of learning, networking, and visioning on April 3, 2018 at the Doctors of BC building in Vancouver.More details about the event will be available soon. In the meantime, if you have questions, contact the Physician Health Program directly at 604-398-4300 or info@physicianhealth.com.
- File Sharing Guidelines
-

What are the guidelines for setting up a shared space for documents to be accessible to hospital-based working group members, project leads and physicians leads who may be at different locations?
You will need to determine what documents are appropriate to be posted on a public-facing website, and what are not appropriate to share – because they contain, for example, confidential information such as personal names and contact information, detailed minutes with sensitive discussions or decisions, strategies, or financial information.
Click here for an overview of guidelines, as well as recommended file sharing tools reviewed by the Doctors Technology Office.
- Privacy Toolkit for Physicians
-

Personal Information Protection Act (PIPA) obligations for physicians: Doctors of BC has collaborated with the Office of the Information and Privacy Commissioner and the College of Physicians and Surgeons of BC to create a privacy toolkit that supports physicians to comply with the Personal Information and Privacy Act (PIPA) to maintain patient confidentiality.
While the guidelines relate primarily to patient care in practice – they may also be applicable to project teams and physicians working on Facility Engagement activities that are related to patient care, or involve patients. Some (but not all) examples include: telehealth video conferencing, secure texting, web-based applications, and data tracking, collection and evaluation.
The toolkit is divided into bite-sized modules for easier review. To get started, read the one-page fact sheet and watch the navigating the toolkit video.
- FEMS Quick Tips - Sessional Rate Increase
-
Physician Sessional Rate Increase: On February 1, 2018 and again on April 1, 2018 the sessional rates for physicians will increase. When submitting claims in FEMS, please make sure that you select the correct date in the ‘Date of Activity’ field. Your sessional rate is dependent upon the date you participated in the activity, not the date you are submitting your claim.
Specialists
To Jan. 31, 2018 - $149.57 per hour
As of Feb. 1, 2018 - $157.00 per hour
As of April 1, 2018 - $157.79 per hour
GPs
To Jan. 31, 2018 $126.80 per hour
As of Feb. 1, 2018 $133.10 per hour
As of April 1, 2018 $133.77 per hour

