FACILITY ENGAGEMENT OVERVIEW & FAQS
Facility Engagement is a BC-wide initiative of the Specialist Services Committee, one of four joint collaborative committees of Doctors of BC and the Government of BC.
It fosters meaningful consultation and collaboration among facility-based medical staff and health authorities on shared priorities that improve patient care and the work environment, while strengthening communication, relationships, and effective processes for working together. It aims to:
- Improve engagement within and amongst MSAs.
- Improve MSA and health authority engagement.
- Enhance the MSA collective voice in health system planning and decision making.
Why are we engaging? Strong engagement among physicians and health organizations supports high quality health care, improving patient outcomes and lowering costs. It also supports effective change in health care. When we work together, we solve problems faster, make better decisions, and achieve more.
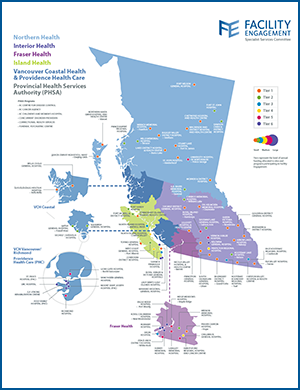
Facility Engagement quick facts
• 6 Health Authorities
• 76 Medical Staff Associations (MSAs)
• 85 facilities and 6 provincial programs
• 2700+ engagement activities
• 6500+ physicians have engaged
Facility Engagement across regions
Across Fraser Health
Across Interior Health
Across Island Health
Across Northern Health
Across PHSA
Across Vancouver Coastal Health & Providence Health Care
---------------------------------------------
Facility Engagement in action
knowledge.facilityengagement.ca

FREQUENTLY ASKED QUESTIONS
- What is Facility Engagement?
As an initiative of the Specialist Services Committee, Facility Engagement was created in 2014 to support medical staff working in facilities across BC to participate in health care planning and solutions.
It creates pathways to meaningful collaboration among medical staff and health authorities on shared priorities, ultimately to improve the delivery of patient care and the clinical work environment.
- It brings clinical and organizational voices together to build relationships, open communication, and mutual understanding as a foundation for strong engagement.
- It creates effective processes, structures, and opportunities for solving problems, planning improvements, and making decisions together.
- It pays medical staff for their time to lead, manage, and participate in local and regional engagement activities with their health authorities – and to hire expertise to support them.
Engagement is defined as…
- A process for making better decisions that incorporates the interests and concerns of affected partners and meets the needs of the decision-making organization.
- An opportunity to strengthen relationships, share information, and build mutual understanding and consensus around shared priorities.
- Why engage?
Physicians and health authorities care about the same things and share many of the same challenges. We can’t solve them without each other.
- Shared priorities: Timely patient access to appropriate, safe, quality care; efficient care delivery, a healthy workplace.
- Shared challenges: More patients, more complex patient care needs, not enough time, scarce resources, and system pressures.
When we work together, we solve problems faster, make better decisions, and achieve more.
- We think bigger, and discover new ways to be efficient, save costs, and maximize resources.
- We share the load to lift burdens, and to create lasting change that matters.
With a path to solve problems and make improvements, each partner benefits:
- Physicians can work more effectively to get patients the right care, safely – and in healthier ways to avoid burnout.
- Health authorities can better manage hospital and patient pressures, and meet responsibilities for lower cost, effective care within budget constraints.
- Who's engaging?
Two main groups are engaging:
1. Physicians and other medical staff, representing a voice for what is needed for patients:
- With a deep understanding of quality, safety, and efficiency of care delivery; initiators of clinical activities and decisions; and a central role in health system expenditures.
2. Health authority leaders and administrators working at local and regional levels, representing a voice for what is possible to achieve in the organization:
- With responsibility for operations, budgets, resources, people, teams, and infrastructure; and deliverables & accountabilities to health authority boards and government.
Participation in Facility Engagement is open to:
- All health authority facilities and programs with acute care beds.
- Specialist and family physicians with privileges in BC facilities who are members of the medical staff and non-physician medical staff members (nurse practitioners, midwives, and dentists).
- Other physicians who are not members of the medical staff, such as community doctors.
- Allied Health providers who are invited to participate by the MSA.
- Medical staff can participate in engagement activities ranging from leadership, to meetings with health authorities, to leading and implementing projects.
- Local medical staff associations (MSAs) manage engagement funds and local engagement activities on behalf of their members, and in partnership with their health authorities.
Facility Engagement participants (2016 – 2025)
- 76 active MSAs (most starting in 2016-17) in 6 health authorities
- 85 acute care facilities and provincial programs represented in 6 health authorities
- Northern Health: 17 MSAs & 17 sites
- Interior Health: 22 MSAs & 23 sites
- Island Health: 11 MSAs, 13 sites
- Fraser Health: 11 MSAs, 12 sites
- Vancouver Coastal Health (including Providence): 9 MSAs, 12 sites
- PHSA: 6 MSAs, 6 provincial programs (BC Centre for Disease Control, BC Cancer Agency, BC Children’s and Women’s Hospital, Concurrent Disorder Providers, Correctional Health Services, Forensic Psychiatric Centre)
- What are its goals?
Facility Engagement aims to foster meaningful consultation and collaboration among MSAs and BC health authorities on shared priorities to achieve these outcomes:
- Improve engagement within and amongst MSAs – with opportunities to connect, identify and set collective priorities, work on projects together, and communicate with each other and the health authority.
- Improve MSA and health authority engagement – through increased and effective communication and interactions between MSA leaders, medical staff, and health authority leaders to co-identify shared priorities and collaborate on developing and implementing solutions.
- Enhance the MSA collective voice in health system planning and decision making – through greater involvement in health service planning and decision-making.
To achieve its goals, FE:- Provides funding and resources to medical staff associations (MSAs).
- Supports local and regional structures and processes for effective interactions between health authorities and MSAs.
- Works with health authority leaders to support shared understanding and partnership opportunities with MSAs.
Key elements include:- Improved opportunities for physicians and health authority leaders to work together to share knowledge and make informed decisions that improve patient care, the physician experience, and the cost-effectiveness of the health care system.
- Opportunities and support for physicians who work at facilities and are members of the medical staff to develop a meaningful voice, and increase involvement in local activities that affect their work and patient care.
- Funding to support activities that involve physicians in decision-making, to pay for their time in activities, and to hire expertise to support them (e.g. a coordinator for administrative support; an analyst to track issues, develop business cases and manage projects; a physician lead to support engagement activities).
- Improve engagement within and amongst MSAs – with opportunities to connect, identify and set collective priorities, work on projects together, and communicate with each other and the health authority.
- How does the Facility Engagement Initiative work?
Facility Engagement is part of BC’s Physician Master Agreement (PMA) between the Ministry of Health and Doctors of BC, and an initiative of the Specialist Services Committee.
- It was initiated in 2014, in response to:
- Low levels of engagement and influence in BC’s health care system among physicians.
- The need for effective structures, processes, and resources for physicians and health authorities to plan and make decisions together affecting patient care and the clinical workplace.
Doctors of BC, the Ministry of Health, and six health authority CEOs across BC signed a Memorandum of Understanding on local and regional engagement, committing to: Memorandum of Understanding (MOU) on Regional and Local Engagem
- Strengthen communication, relationships & engagement between facility-based physicians & health authorities through medical staff association structures.
- Increase meaningful physician input and involvement in health authority planning and initiatives that directly impact their work environment and patient care delivery.
The Specialist Services Committee is overseeing the initiative and distributing funding. Funding is administered through a physician society or alternative structure established at local facilities.
The provincial initiative maintains flexibility for activities to be tailored to each facility at the local or regional level.
- It was initiated in 2014, in response to:
- Provincial agreements
- SSC Facility Engagement Working Group
Who is the Specialist Services Committee (SSC) Facility Engagement Working Group (FEWG) and what is their role?
The SSC FEWG consists of one health authority and one Doctors of BC physician representative from each of the 5 health authority regions, as well one Ministry of Health and one Doctors of BC physician co-chair.
The group meets 5-6 times a year and provides provincial oversight and governance for the FE initiative. It oversees the implementation of the Memorandum of Understanding on Regional and Local Engagement (MOUO), reviews MSAs' annual review submission packages, advises on funding guideline changes, develops the FE Evaluation Program, facilitates involvement of Health Authorities in the implementation of the MOU, and more.
To keep you informed about what is happening at the provincial level to better support your work and strategic decision-making, SSC FEWG meeting summaries will be reinstated. These summaries provide insight into how and what decisions are being made at the provincial level for the Facility Engagement Initiative.
SSC FE Working Group Meeting Summaries
- What is a Medical Staff Association (MSA)?
MSAs represent the voice of medical staff in BC hospitals and provincial acute care programs.
- Medical staff include physicians and surgeons, nurse practitioners, midwives, and dentists.
- Part of the MSA role is to oversee local Facility Engagement governance, funds, and engagement activities on behalf of their medical staff members, and in partnership with their health authorities.
- Physician Master Agreement negotiated funds and resources provided through Doctors of BC / Specialist Services Committee (SSC) support MSA engagement activities, with guidelines and goals for using the funds.
- MSAs are not governed or directed provincially by Doctors of BC / or the SSC.
- Instead, MSAs exist under their health authority medical staff bylaws and rules with a mandate to provide a voice to the medical staff, promote and advance medical staff involvement in the provision and planning of medical services at their facilities, and to elect officers.
- MSAs and their health authority partners are supported in their engagement work by provincial Engagement Partners and the Facility Engagement team at Doctors of BC.
- What are the roles of engagement participants?
Roles: Overall, MSAs and health authorities work with each other on mechanisms for effective communication / interactions with medical staff.
Go to roles in full: MSA executive roles, health authority roles, support roles
MEDICAL STAFF ASSOCIATION (MSA) ROLE: Represents the voice of all medical staff members.
Role in facilities:
- Represents collective and individual member views.
- A forum to inform and connect.
- Raises significant matters with administration, LMAC, HAMAC.
- Engages medical staff locally on program and resource planning.
- Supports effective communication between medical staff, medical & operational leaders.
Role in Facility Engagement:
- Maintains governance and decision-making structure.
- Manages/reports on FE funds.
- Consults, involves and collaborates with health authority on local engagement initiatives.
- Manages engagement activities representing medical staff priorities.
HEALTH AUTHORITY ROLES: Multi-level responsibility for medical care and operations.
Role in facilities:
- Clinical governance, quality assurance, credentialing & privileging.
- Medical staff CPD.
- Managing operations, budgets and resources (e.g. infrastructure, HHR, contracts).
- Accountable to HA Boards and MOH mandates.
Role in Facility Engagement:
- Consults, involves, and collaborates with medical staff on MOU commitments.
- Appropriate information to medical staff to effectively engage & consult.
- Partners with MSAs on potential funding proposals aligned with FE goals.
SUPPORT ROLES
- How does the funding work?
FEI funding is provided through the Specialist Services Committee (SSC) to MSAs based on the number of acute care beds their facility or program supports – with provincial guidelines, and with flexibility for local implementation.
- It pays medical staff members for their time to oversee, plan, lead, and participate in local and regional engagement activities, and to hire operational and administrative support.
- MSAs can optionally extend funding for participation in engagement to medical staff who are not privileged at the facility (such as community-based doctors), or Allied Health providers.
- The SSC Facility Engagement Working Group provides provincial oversight for the FEI. It is comprised of Doctors of BC MSA physicians and Ministry and health authority representatives.
- At the local facility level, funding is governed and managed by Medical Staff Associations (MSAs) for priority activities set out by medical staff, with flexibility to be tailored to each facility.
- Some larger MSAs have set up non-profit physician societies to hold and manage FEI funds, while other smaller, unincorporated MSAs have their funds held and administered through the Facility Engagement Services Company (FESC).
To qualify for and receive annual funding, medical staff must have:
- A governance and a decision-making structure that will represent the MSA members in the facility.
- The ability to receive, account for, and report on expenditures.
- General agreement to proceed with health authority representatives at the start of the process.
To find out if/how your MSA is involved, contact your medical staff president and/or local MSA administrator or e-mail engagement@doctorsofbc.ca.
- What kinds of activities are underway?
A wide variety of activities are underway across BC. A few examples include:
- Leading clinical improvement projects across departments/interdisciplinary teams.
- Working on hospital-wide priorities like access and flow, culturally safe care, and hospital redevelopment.
- Supporting recruitment & retention.
- Supporting regional priorities like medical staff engagement in EHR implementation in facilities, planetary health, and patient transport.
- Addressing medical staff wellness and burnout.
For more activities from across BC, see:
- What are examples of new processes to engage?
Examples of enhanced for new structures & processes include:
- MSA executive and working group meetings.
- Participation of MSA executives or representatives at local and regional health authority meetings (e.g., medical advisory committees, quality of care).
- Local and regional MSA-health authority meetings and events to build relationships, share knowledge, successes and learnings, and co-identify and collaborate on shared priorities.
- More physician and health authority leader dyads to align strategic priorities and work directly together on plans and initiatives.
- Increased communication channels for communication and two-way feedback with members, and greater transparency.
- What is the value of Facility Engagement?
Facility Engagement is creating structures, processes and opportunities that did not exist in the past for connection, communication, dialogue, and meaningful collaboration:
- Triad relationships: operational + elected medical staff leaders + medical staff = solid foundation for change.
- Involves and incorporates the concerns of affected groups.
- Aligns medical staff and organizational strategic goals.
- Meets the needs of the organization and providers.
- Funds physicians to be part of planning and solutions.
Facility Engagement is building team culture in hospitals through an increased and shared understanding of respective priorities and needs, new trusted and supportive relationships:
- Builds mutual consensus.
- Demystifies pressures & roles.
- Moves away from “us vs. them”.
- More proactive, less reactive.
Improves workplace culture: wellness, connection, energy; supports recruitment and retention.
- What is changing and improving?
Progress: emerging success factors (evolving, with more work to do)
- Effective relationships and processes to solve problems together.
- Physicians and health authorities contribute to mutual plans and decisions.
- Improved patient care and the clinical workplace.
- Physician influencing and leading system change.
Increased engagement among medical staff
- Communication, collegiality.
- Collaboration for patient care across clinical areas and facilities.
Increased engagement between MSAs and health authority leaders
- Communication, collaboration & teamwork.
- More relationships & progress with local medical leaders.
Increased alignment of medical staff and health authority strategic priorities
- MSA/Senior leader dyad partnerships and collaboration around shared priorities.
Increased contributions to patient care through 1100+ Facility Engagement projects, focusing on patient care improvements/innovations.
Increased contributions to facility culture (2023 Evaluation Survey)
- 66% of physicians agree or strongly agree that MSA activities have helped improve facility culture.
- 72% of Health Authority medical and operational leaders strongly agreed/agreed: MSA activities have helped improve facility culture.
- 63% of Health Authority medical and operational leaders strongly agreed/agreed: MSA activities have helped improve the delivery of patient care.
- FE Evaluation Reports
UBC Provincial Evaluation 2015-2019
- FE Interim Evaluation Stage One Summary
- FE Provincial Evaluation Report Two Page Summary
- FE Provincial Evaluation Final Report

Ference Provincial Evaluation 2020-2021
- FE Evaluation 2.0 Overview
- FE Evaluation 2.0 Interim Report Executive Summary 2021
- FE Evaluation 2.0 Interim Report 2021
- FE Evaluation 2.0 Collective Story Report 2021
- FE Evaluation 2.0 Findings and Opportunities 2021
- FE Evaluation 2.0 Final Report Executive Summary
- FE Evaluation 2.0 Final Evaluation Report and Video Presentation
- FE Evaluation 2.0 Collective Story Report
- FE Evaluation 2.0 Action Plan

Ference Provincial Evaluation 2022-2024
- FE Evaluation 3.0 Survey Data Technical Report
- FE Evaluation 3.0 Interview Technical Report
- FE Evaluation 3.0 Final Report and Video Presentation
- FE Evaluation 3.0 Learnings and Opportunities